THE ‘STATISTICALLY significant’ increase in maternal deaths reported on Thursday by MBRRACE-UK is a tragic indication of a lack of government investment in maternity services, according to the Royal College of Midwives (RCM).
Many of the deaths cited in the report are linked to mental health issues and although improving, there are continuing inequalities in outcomes for Black and Asian women when compared to their white counterparts and for women living in deprived areas.
Promised investment must be funnelled more quickly to where it is needed in key areas such as staffing and ongoing training to stem this tragic rise, says the RCM.
Serious and growing midwife shortages across England mean staff are often pulled away from antenatal and postnatal care to cover labour and birth.
England is currently at least 2,000 midwives short of the numbers needed and this is worsening month by month.
‘With many of the maternal deaths cited in the report linked to the postnatal period and lack of access to perinatal mental health services, the RCM says maternity services must have the right staffing across the board to ensure safe care for women throughout and beyond pregnancy.
Senior midwives across the country are having to make hard choices about where they deploy their staff because of the government’s failure to act quickly enough and this is hitting access to safe and personalised care, says the RCM.
Gill Walton, Chief Executive of the RCM, said: ‘Any rise in maternal deaths, however small, is deeply worrying and we are moving backward not forward.
‘Governments must focus efforts on the crucial areas where women are being let down and not getting the care they deserve and should expect.
‘They cannot expect services to keep robbing Peter to pay Paul. This is having disastrous consequences for women and families and is impacting staff. We have overstretched midwives and maternity services that have been trying to do too much, with too little, for far too long.
‘This should be a time of great joy for women and families, but tragically for some, it is a time of heartbreak. For all of us, women and their needs should come first and be right at the heart of everything we do.
‘Serious staffing shortages within midwifery, obstetrics and related health professions are undermining the ability of maternity staff to deliver the safest possible care.
‘We have a burnt-out and fragile maternity workforce who often cannot even do crucial mandatory training because of shortages and pressures.
‘The sheer will and commitment of midwives, maternity support workers and their colleagues is keeping services afloat. It is clear though that their incredible dedication is not enough and they must be supported to deliver the care they so desperately want to.
‘This is fundamentally a failure of policy makers and the government to get funds quickly to where they are needed at the frontline of care. We have been raising this issue repeatedly and we must see this change rapidly to prevent avoidable deaths.
‘The RCM is at the forefront of efforts to make care for women better and safer and to tackle inequalities in maternity care.
‘However, this has to be backed up with government action to reverse some of the deeply worrying findings in this report,’ says the RCM.
The College is collaborating with many organisations to support midwives, MSWs and other maternity staff to deliver the safest possible care including its involvement in the MBRRACE-UK reports. Among other key RCM joint initiatives are the Avoiding Brain Injury in Childbirth programme, the Tommy’s National Centre for Maternity Improvement and Each Baby Counts projects.
- A record number of patients had to wait to be seen in A&E departments in October, NHS England figures show.
More than 550,000 patients were waiting more than four hours, up from 492,000 in September, and the highest proportion on record.
The Society of Acute Medicine warned the situation was ‘unacceptably poor’ and likely to deteriorate further.
The NHS said it faced the busiest October ever in A&E and for the most serious ambulance call-outs.
Separate figures showed the number of the sickest patients having to wait a long time for a spare hospital bed also increased sharply in England.
In October, 43,792 patients had to wait at least 12 hours in A&E after a decision to admit to a ward had been made, up 34% from 32,776 in September, and the highest number in records going back to August 2010.
The average response times for ambulances rose across much of the country.
Outside the capital, response times for a category two emergency, such as a stroke or suspected heart attack, rose in almost every English region.
In the West Midlands, the average time to reach those patients increased to one hour, eight minutes in October, up from 45 minutes in September, and well above the 18-minute target set out in the NHS constitution.
Dr Tim Cooksley, president of the Society for Acute Medicine, said all parts of the NHS were ‘unquestionably struggling’.
He added: ‘This latest set of performance data shows that standards are at an unacceptably poor level for both patients and staff, with an expectation that this will deteriorate further over the winter months.
‘Pressures are at unsustainable levels and the results are scant justice for acute care staff who continue to strive to deliver a reasonable quality of care. Morale for patients and staff is low with little expectation of short-term improvement.’
There has also been a sharp rise in long waits for cancer therapy in the past four years, BBC analysis shows.
The number waiting more than the 62-day target time for therapy in the past year has topped 69,000 across England, Northern Ireland and Scotland, twice as many as the same period in 2017-18.
Steven McIntosh, of Macmillan Cancer Support, said: ‘The NHS doesn’t have the staff it needs to diagnose cancer, to deliver surgery and treatment, to provide care, support and rehabilitation.’
He warned there would be further delays and disruption if NHS spending did not at least rise in line with inflation in the Chancellor’s November budget.
Separate data showed the number of people in England on a waiting list to start routine treatment, such as a knee replacement or cataract surgery, has also risen to a new record high.
A total of 7.1 million people were waiting to start treatment at the end of September, NHS England said.
That is up from seven million at the end of August and is the highest number since records began in August 2007.
A total of 401,537 people had been waiting more than 52 weeks to start their treatment, up from 387,257 in August.
Meanwhile, commenting on the nurses’ strike vote, shadow health secretary Wes Streeting said there were no strikes during Labour’s time in office and argued that ‘if we were in office today, we would be talking with the RCN and doing everything we can to prevent these strikes.’
Streeting added: ‘Government ministers spent the summer dodging calls and requests for meetings from the Royal College of Nursing. It is unacceptable negligence.
‘The Conservatives have stopped governing and it is nurses and patients who will be made to pay the price.’
He told LBC’s Tonight with Andrew Marr on Monday: ‘I’m concerned, I think lots of people are concerned about the impact of disruption. That’s still a disruption to patients, which I think is unacceptable.’
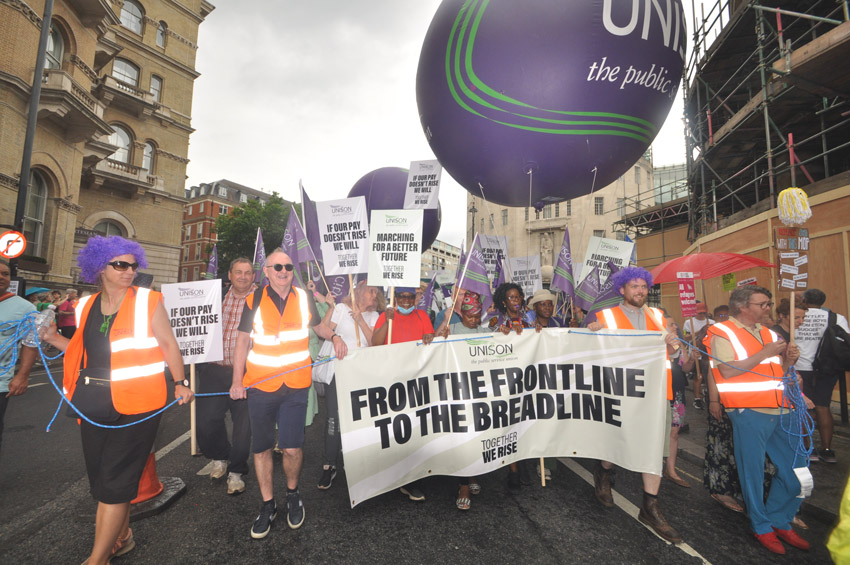
Head of health at Unison Sara Gorton described the outcome of the union’s strike ballot as a ‘loud wake-up call to the government’ and warned that now is the time for ‘swift action to avoid a damaging dispute’ with other NHS employees considering a strike.
She added: ‘NHS managers are fighting a losing battle. They know pay and the lack of staff are the main reasons why health workers are leaving at alarming rates. The NHS cannot keep patients safe without improving staffing levels. Boosting pay is a crucial first step in dealing with the NHS workforce crisis.
‘The government must put pay right to spare the NHS, its staff, and all those relying on its care, from a dispute no one wants to see.’
Tory health secretary Steve Barclay said: ‘We deeply regret that some union members have voted for industrial action.’
Privately, sources at the Department of Health and Social Care claim that the RCN is seeking a 17.6% rise, which if applied to all NHS staff covered by Agenda for Change – paramedics, physiotherapists, cleaners and porters, for example – would cost £9bn. That £9bn would be 6% of NHS England’s £152.6bn budget this year, sources point out.