THE NHS won’t survive without immediate steps to bolster our workforce, doctors union the British Medical Association (BMA) warned on Monday.
Responding to the Tory government’s Delivery plan for recovering urgent and emergency care services, Professor Phil Banfield, chair of BMA council, said: ‘The NHS cannot afford to wait two years for the fraction of help that the government has proposed in this plan today.
‘If the NHS has any chance of surviving that long, then we need to see immediate funding as well as steps taken to retain and boost our workforce.
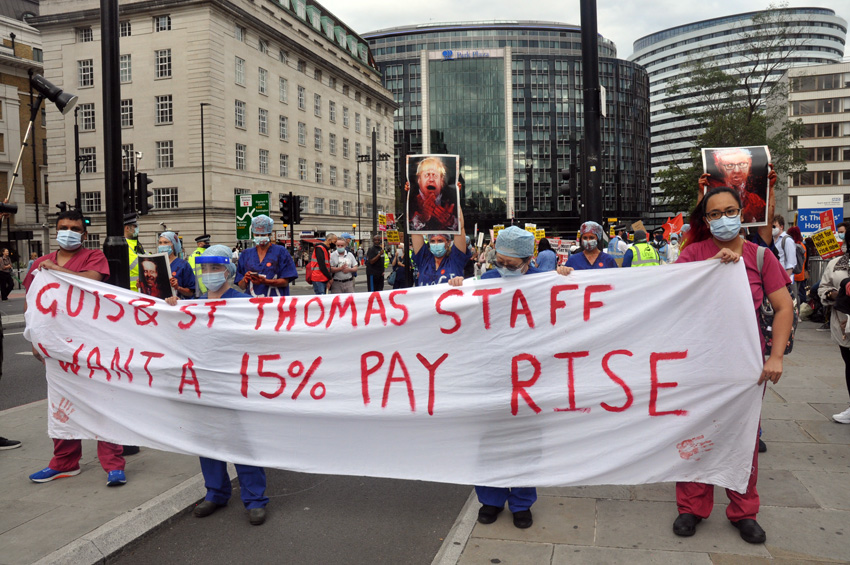
‘People aren’t leaving the NHS solely because they struggle to work flexibly, as this plan suggests. They’re leaving because they aren’t paid fairly, are subject to punitive pension taxation, and don’t feel valued.
‘It’s therefore, laughable that with 133,446 vacancies across the NHS, the government still hasn’t addressed the workforce crisis. They may be able to source more ambulances, but who is going to staff them?
‘The only mention of active recruitment is in relation to NHS 111 – and that comes from recruiting healthcare workers from other, already severely understaffed parts of the health service. Moving existing staff and finances around is not the way to fix this.
‘The irony of looking at new ways of delivering care in the community is not lost on hardworking GPs who have offered to sit down to negotiate delivery of better services.
‘Virtual wards, for example, are an attempt to free-up capacity in hospitals, but these patients still need monitoring, which requires someone to do this. It’s the same problem, just in a different place.
‘Without a dedicated workforce and significant resource for this, now, it’ll likely fall to already-overworked GPs and their teams to pick up the workload, pushing up waiting times in general practice and jeopardising patient safety even further.
‘As things stand, there’s no guarantee ambulances will be able to reach patients if their conditions deteriorate, and we urgently need to see capacity improved in social care. Doctors are repeatedly looking to innovate, but must be facilitated and funded to do so.
‘Today’s plan shows that the government still doesn’t understand the health and care workforce crisis.
‘The BMA does, and will be publishing its own emergency plan in the coming days, which puts valuing healthcare workers front and centre, with immediate solutions like addressing pay restoration and punitive pension taxation. Only then can we retain and attract the workforce we need to deliver the care our patients deserve.’
Also commenting on the government’s proposals to boost NHS emergency care, the Unison union’s head of health Sara Gorton said: ‘There’s nothing to deliver the urgent retention plan needed to stop staff leaving jobs in the NHS. Nor is there anything about boosting pay to prevent the current industrial unrest from spreading.
‘Without halting further strikes over pay and staffing, it’s difficult to see how this plan will be delivered. Particularly with precious little new funding from the Treasury.
‘The success of the NHS begins and ends with its employees. No plans to deal with waiting times and handover delays stand a chance without tackling staffing shortages.
‘To do that, ministers must begin genuine pay talks with unions right away and make a commitment to a proper wage boost.’
Responding to Tory Chancellor Hunt’s speech last Friday about driving UK economic growth, Unison general secretary Christina McAnea said: ‘Jeremy Hunt’s grand vision for the future completely ignores vital public services.
‘The Chancellor holds the key to unlock the damaging health pay dispute and rebuild the NHS, but he’s not even trying.
‘No plan for the economy can succeed unless the government also focuses on essential services.
‘Paying proper wages will halt the staff exodus and mean there’s more money to spend in the local high street.’
- Thousands of NHS staff across the UK are facing pay cuts because of a change in Covid sickness policy.
Monday night’s BBC Panorama broadcast found that between 5,000 and 10,000 NHS workers are off sick with long Covid, and unions are accusing the government of failing to support health staff who worked during the coronavirus pandemic.
The government says the Covid-19 public inquiry will examine these issues when it begins taking evidence in May.
Changes to special sick pay rules introduced during the pandemic mean that some NHS staff unable to work due to long Covid may soon no longer receive full pay.
Enhanced provision ended last year. Many had a six-month transition, so expect their wages to go down soon.
Rachel Hext, a 35-year-old nurse at a small community hospital in Devon is hoping to get better after developing long Covid as she has been unable to work for two years, but is not sure she will lever be the same again.
In October 2020, she was caring for Covid patients, but a few days later, she tested positive. Her symptoms include chest pain, brain fog, fatigue, joint pain, allergies, heart problems, sinus issues and hearing loss.
Hext is still on full pay but a change in sickness rules means her salary is due to be cut in half at the end of February.
She says she will be £1,000 a month worse off.
She has applied for an NHS Injury Allowance, which could top up her pay, but doesn’t know if she will get it.
The Torbay and South Devon NHS Foundation Trust says it can’t comment because there is a legal claim, which it is defending.
The trust’s chief executive, Liz Davenport, said: ‘The health and wellbeing of our staff is our priority, and we are extremely grateful to all our colleagues in the NHS and care services who worked tirelessly during the pandemic to care for our patients.’
But Hext is now really worried about money. She said: ‘I do appreciate the NHS can’t pay us forever, but there’s hope we can actually bring something back to the NHS again.’
At the start of the pandemic, the government brought in special Covid sick pay for staff directly employed by NHS Trusts.
This meant that, if they got Covid, they would get full pay, however long they were off work.
This didn’t include everyone. For example, GPs were not covered.
It was a temporary measure and the scheme ended last summer.
There is some local discretion and the rules may vary depending on length of service and where people work in the UK.
But essentially, standard sick pay rules have come back for NHS staff.
This means that some people have already seen their pay go down, with more to follow soon.
The NHS in England and Wales do not publish overall numbers for showing how many staff are off sick with long Covid.
Northern Ireland’s Department of Health told the BBC its most recent figures show 0.6% of its health and care staff are off because of long Covid. In Scotland it’s 0.3%.
If these rates are reflected across the UK, it could mean that between 5,000 and 10,000 staff absent because of long Covid, and some face losing their jobs.
Professor David Strain, chair of the Board of Science at the BMA, says this makes him ‘genuinely angry’.
He told the BBC’s Panorama programme: ‘We’ve got a group of people that have put themselves forward to look after the population, they’ve been left with an illness and they’re not being supported.
‘They’re just in a no man’s land.’
He believes that health workers with long Covid should be allowed to focus on their recovery without money worries.
Layla Moran MP, chair of a cross-party group of politicians looking at how the pandemic was handled in the UK, says other countries have already designated Covid as an occupational disease, entitling those affected to financial support.
She said: ‘We are falling behind our peers in our recognition of this as a real disease that needs proper recognition and compensation.’
NHS guidelines encourage managers to support staff to return to work, with options like phased returns.
A government spokesperson said: ‘The Covid-19 inquiry has been set up to examine the government’s response to the pandemic and we will respond openly and transparently to the inquiry.’
And the government ‘accepts that long Covid is having an impact on the NHS, contributing to workforce inactivity.’
The inquiry will start hearing evidence in May. It has a huge scope and could last for years.