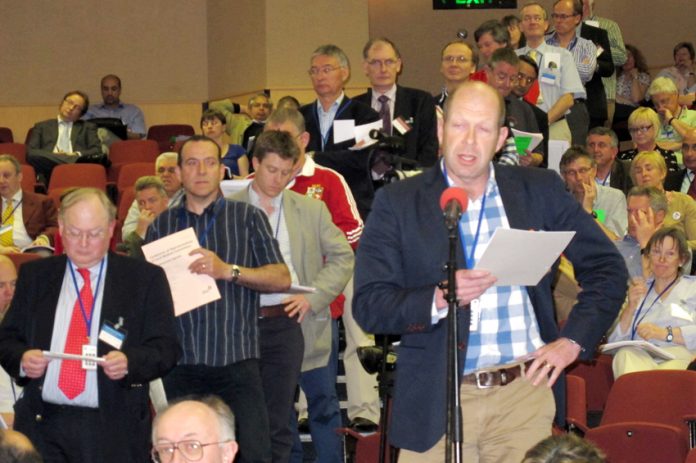
GPs meeting in London on Thursday reacted angrily to the government’s cuts and drive to privatise, and press and government propaganda blaming GPs for all the ills of the NHS.
The first motion to be heard at the BMA Conference of Representatives of Local Medical Committees, stressed that general practice gave ‘superb value for money’ but GPs are ‘concerned that as funding falls as a share of total health spending, governments are more interested in a cheap option’.
Motion 7: ‘The NHS in Crisis’ was moved by Grampian GP Denise McFarlane, who said: ‘The average GP is a low-cost option. We fear plans to increase nurse practitioners and other cheaper options.
‘The public have confidence in doctors, less than two in ten trust politicians.
‘The government tend to throw more at us but with no extra funding.’
She concluded: ‘Investing in general practice means we can rise to the challenge again, again and again.’
Speaking for the motion, Gwent GP Mike Griffiths warned: ‘The government is not interested in funding us, the government is only interested in creating challenges.
‘The government is only interested in privatising the NHS and taking it off the Budget.’
Calling for a unanimous vote, Beth McCarron-Nash from the General Practitioners Committee (GPC) moved Motion 8: ‘NHS Reforms/Health and Social Care Act’ which warned ‘the NHS organisational reforms and administrative burdens’ resulting from the Act.
‘(i) are putting services and quality patient care at risk;
‘(ii) will further widen population health inequalities and compromise the health of the nation;
‘(iii) will seriously threaten core general practice and will destroy the viability of practice.’
She said: ‘GPs have little more control over services now than we did before.
‘We have the accountability without the power. Competitive tendering is not choice. Patients have been told we’re in charge when we’re not.
‘We must renew investment in high-quality service.’
Cheshire GP Peter Madden told conference that his profession was ‘in the direct firing line’ of the government. He warned: ‘GPs will take the blame for failure.’
He said that issues such as the imposition of contract and pension changes, meant all practices were under severe financial threat.
He added: ‘We have heard about workload problems and the impending workforce crisis. We have the ingredients for a perfect storm.’
Liverpool GP Andrew Taylor said: ‘Successive governments have redirected funds for their agenda to push home privatised care.’
He said there was a mass exodus with the early retirement of older GPs and emigration of younger ones and warned that ‘general practice is dying’.
He concluded by imploring the conference: ‘Don’t let deceitful, duplicitous politicians and governments destroy the GP jewel in your NHS crown.’
Newcastle GP Gerard Reissmann maintained that the government was ‘destroying the NHS’.
He said that ‘services were handed over before the Bill came in’ and cited the example of the private takeover of Hinchingbrooke hospital management.
He warned: ‘It will be the poor who will have a limited access to services.’
He insisted: ‘This isn’t our doing, we are watching this car crash and we are saying this is happening.’
GPs voted almost unanimously, with one abstention, for Motion 10: ‘That conference believes that the government wishes to privatise the NHS and demands that it is made public knowledge.’
Mover Francesco Scaglioni, Cornwall and Isles of Scilly, told conference: ‘Cameron said there would be no top-down change to the NHS. It wasn’t in the Tory manifesto.|
‘The NHS budget is being opened up to clients of Monitor.’
Scaglioni alleged: ‘£20,000 was paid into the office of (former health secretary) Andrew Lansley the day the bill was announced.’
Moving Motion 12: ‘Francis Report’, Kent GP Gaurav Gupta called for the GPC to drive a return to patient-centred holistic care and renounce target-driven cultures in light of the events in Mid Staffordshire.
Dr Gupta told the conference that events at the Mid-Staffs hospital trust were caused not by ‘lack of compassion but lack of time and resources’.
He said general practice was ‘at breaking point’ and the only way to save the NHS was to invest in primary care.
Although GPs maintained their concern for patients when they were admitted to hospital, he argued they could not be held clinically responsible for their care while they were inpatients.
‘GPs cannot and should not be held responsible for care in the hospitals. Being in two places at the same time is beyond us,’ he said.
Cambridgeshire GP Alan Mills said there was a mismatch between the resources available and the needs of the system.
He said GPs were doing ‘more and more for less and less’ and this was ‘threatening the very viability of our practices’.
He added: ‘If we do the same for less, the quality of our services and our practices will suffer.’
Derbyshire GP John Greville argued: ‘We are seeing more and more patients with more and more complex problems.
‘We need more time. We must say loud and clear that we need time. We need more resources in primary care.’
London GP Eleanor Scott called the events at Mid Staffordshire ‘a horror and a tragedy’ of our times and said that nothing similar must happen in primary care.
She said the government must understand that GPs are ‘already suffering from institutional exhaustion’.
She concluded: ‘A Mid Staffordshire in general practice? Not on our watch.’
GPs went on to vote unanimously to demand an independent inquiry into the NHS 111 ‘debacle’.
They also demanded a government-commissioned probe into the ‘wholly inappropriate’ use of the least-qualified people for triaging calls made to the urgent non-emergency phone line.
The BMA local medical committees conference heard accounts from GPs about the botched implementation of the service in March this year.
Manchester GP John Hughes described the implementation as an ‘omni-shambles, a complete disaster, a complete waste of public money’.
He said he had seen a confidential report into the implementation of NHS 111 which blamed insufficient call handlers, poorly trained staff and inadequate governance.
Dr Hughes added: ‘The finding of the pilot had been ignored. There was extreme pressure for a soft launch.
‘We warned in the time running up that this was unsustainable…We need a public inquiry into this.’
Fellow Manchester GP Ash Bakhat described how the launch of the service in the North West in late March was met with silence when calls did not come through to GP practices from the triage service for hours.
He said the out-of-hours service later reported around a third fewer calls than usual. He added there was then a ‘scramble’ to get back on track when practices were forced to switch back to their usual methods of call handling.
Norfolk GP Nick Morton suggested the NHS 111 call centres should have a GP present to do a ‘sense check’ on triaging which would also protect NHS resources.
He described the NHS 111 as a ‘Trojan horse’ and said GPs should beware.
Middlesbrough GP Bill Beeby led calls for any inquiry to also include the inappropriate use of the least-qualified people to handle NHS 111 triage calls.
‘In no other area are minimally trained staff expected to deal with the complexity of triage,’ he said.
‘Giving out a phone number for a self-help group is fine but deciding who needs a paracetamol or an ambulance is not a job for triage.’
Kent GP Neil Potter expressed concerns for palliative patients caught up in the system.
‘In the current system in our area there are no special arrangements – they are in the hopeless queue with everyone else,’ he said.
Dr Potter said the service had increased expectations but reduced delivery.
Responding to the debate, GP negotiator Peter Holden said the BMA had repeatedly warned the government not to roll out NHS 111 but it had not listened to concerns that systems were not ready.
‘We want an independent inquiry and that means an external inquiry,’ Dr Holden said.
GPs queued up to speak on a motion calling for urgent action to address the workforce crisis in general practice.
They want to see measures to:
• Promote the recruitment of potential GPs;
• Support the retention of existing GPs;
• Reduce the barriers for GPs returning to practice.
Leeds GP Raj Menon said: ‘General practice is facing a workload and a workforce crisis. We are workload saturated…We need more GPs to be able to cope with the patterns of healthcare in the future.’
Derbyshire GP Peter Williams said two GP partners in his practice had retired in their 50s because they could not take the pressure any more.