THE BMA has responded angrily to threats to GPs issued by the government’s new Chief Inspector of Primary Care, Professor Steve Field, who takes up his position tomorrow.
Field claimed in a newspaper article on Saturday that 10 per cent of GP surgeries ‘aren’t providing appropriate access or quality of care’ and that he ‘won’t hesitate’ to close them down.
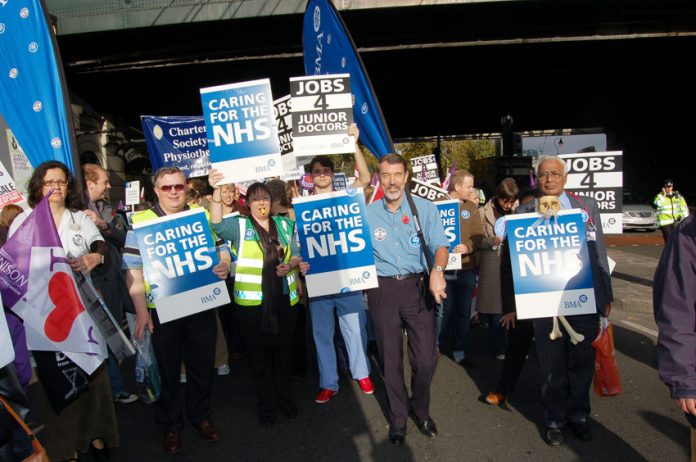
The BMA condemned Field for ‘beginning with a stick approach of threatening to close GP surgeries, with loss of local services to patients’.
In his first interview since being appointed as the NHS’s first Chief Inspector of Primary Care, Field said he ‘would not shy away from using sanctions, including fines and suspensions of surgeries’ licences’.
He said: ‘I will not hesitate at all to order the closure of GP practices that we find to be unsafe, or providing poor access, or which do not care for patients properly or treat them with dignity.’
Field, who is to introduce an Ofsted-style regime of inspections and ratings for GP practices, claimed that ‘10% of the 7,607 GP surgeries in England need to make major improvements’.
Dr Chaand Nagpaul, Chair of the BMA GPC responded: ‘The overwhelming majority of GP practices offer excellent care and have high patient satisfaction ratings.
‘Intense workload pressures, due to the escalating demands of an ageing population and care moving out of hospitals mean GPs are seeing more patients than ever before – 340m in the last year.
‘There are not enough GPs to cope with current demand and in order to provide more services and longer access, there needs to be a massive expansion of GP numbers, staff and premises.
‘There are a number of reasons why a small minority of GP surgeries are failing to provide adequate care, including in some cases working with inadequate resources and premises.
‘Rather than beginning with a stick approach of threatening to close GP surgeries, with loss of local services to patients, we should adopt a systematic approach of enabling improvement in the first instance.
‘The quality of out-of-hours care cannot be divorced from the serious failings and shortcomings of NHS 111 as the first point of contact for many patients.
‘This must be addressed as a priority, as well as supporting an integrated approach for all providers of urgent care out of hours, which should include walk-in centres, minor injury units, ambulance services, A&E and social care.’