A STARTLING new report published by the Queen’s Nursing Institute (QNI) states that during the peak of the pandemic people in care homes were given a blanket ‘Do Not Resuscitate’ DNR order, meaning that if they went into cardiac arrest or stopped breathing they would be left to die.
The report, based on a survey of care workers, managers of care homes and nurses, concludes that elderly and disabled of all ages including disabled younger people were given the DNR orders, in many cases without even consulting the families first.
The report states that one in 10 care home staff were told to change DNR orders for their residents. It was not just the extremely frail and elderly who had their orders changed to DNR but younger people with disabilities as well.
Professor Alison Leary MBE, an expert in healthcare and workforce modelling at London South Bank University, said: ‘10 per cent of the respondents raised an issue, because they were either blanket decisions for whole populations, or they were imposed without discussion with the care home or the family or the residents, and that is really worrying.’
Jonathan Ashworth, the Labour Party’s shadow health secretary, said it was ‘scandalous’ that DNR forms had been used in this way.
Ashworth said: ‘To have left care home residents and staff not just unprotected and exposed to Covid-19 but to have put in place procedures that actively allowed Covid-19 to spread in care homes is an atrocious failure of Boris Johnson.’
QNI said of the survey results: ‘Worryingly, some who responded raised serious ethical and professional concerns, for example GPs, Clinical Commissioning Groups and hospital trusts making resuscitation decisions without first speaking to residents, families and care home staff or trying to enact “blanket” “do not resuscitate” decisions for whole groups of people.’
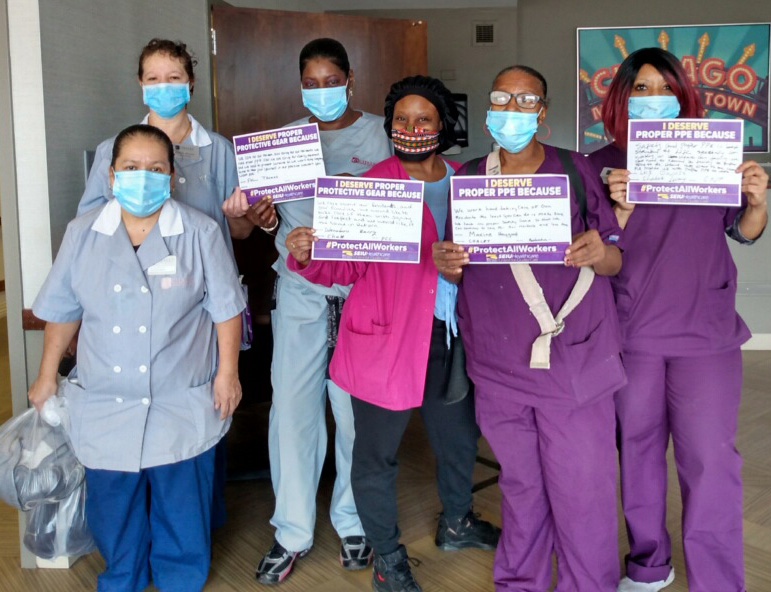
On the issue of a lack of Personal Protection Equipment (PPE) QNI continued: ‘The need for appropriate PPE in care homes is of critical importance in staff and resident safety: 21 per cent of respondents said that their home accepted people discharged from hospital who had tested positive for Covid-19.’
In the key findings of the report QNI stated:
‘• 16 respondents reported negative changes which they found challenging such as “blanket DNACPR” decisions, or decisions taken about resuscitation status by others (GPs, hospital staff or Clinical Commissioning Groups) without discussion with residents, families or care home staff or that they disagreed with some of the decisions on legal, professional or ethical grounds.’